Why Therapist Supervision Matters:
The Hidden Mistakes It Prevents
Research shows therapy supervision barely affects client outcomes. It accounts for less than 1% of variance in therapeutic results. Edward Watkins Jr.'s review of 18 empirical studies about supervision's effect on client well-being raised a challenging question: "If we cannot show that supervision affects patient outcome, then how can we continue to justify supervision?"
The measurable results might look disappointing, yet supervision remains central to therapists' professional routines. This creates an interesting contrast. About one-third of our clients show no reliable improvement in therapy. More concerning, 10% of clients make up 60-70% of behavioral health care costs because they keep using services without getting better. Clinical supervisors provide vital support. They help assess complex cases, develop treatment plans, make ethical decisions, and work through challenges.
Over time, supervision has evolved. It’s moved from old-school mentorship to something much more intentional—something built on trust, accountability, and real conversations.
The Modern Shift
With the rise of:
Virtual therapy
AI tools
Culturally complex cases
Supervision has had to adapt. And thank goodness it did. Because we’ve all benefited.
Why therapist supervision matters more than ever
"Supervision was also seen to drive up the quality of care and has a positive effect on the working environment." — Alison J. Noble, Senior Lecturer in Clinical Education, University College London
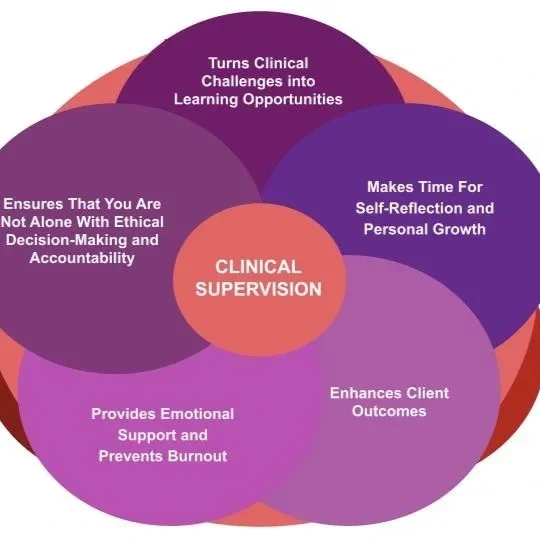
What Supervision Actually Does
Supervision isn’t just a checkbox to keep your license.
Here’s what it really brings to the table:
Normative: Ensures quality, ethics, and safety
Formative: Builds your skills and confidence
Restorative: Supports your emotional well-being and helps you not burn out
These functions are essential—especially when burnout rates are sky-high. Some studies report 21–67% of mental health providers experience burnout.
Supervision gives therapists room to exhale, reflect, and regroup.
And for those of us in private practice? It’s not optional. It’s our lifeline.
See also: Preventing Burnout as a Therapist
The evolving role of supervision in modern therapy
The last decade has transformed supervision from traditional mentorship models to structured approaches that integrate theoretical frameworks and evidence-based methodologies. These changes reflect broader shifts in healthcare education, which now emphasize standardized practices and measurable outcomes. Research shows supervision as a strong contributor to, and potential enhancer of, the supervision process itself.
The COVID-19 pandemic changed how professionals conduct supervision. Healthcare has seen faster growth in telehealth, which pushed supervisors to help supervisees tackle unique challenges from virtual therapy. Many clinical training programs now welcome telesupervision. This allows them to reach clients who might not otherwise get services—especially those in disadvantaged communities.
New technologies like artificial intelligence are starting to reshape supervision practices. One expert states, "AI can make things easier, but it's not at a place where we would like to see it yet from a university view". Supervisors must keep updating their knowledge base to stay current with these technological developments.
The field has become more multicultural-minded alongside these technological changes. Every supervision represents a triadic multicultural relationship. Variables like gender, race/ethnicity, sexual orientation, and religion/spirituality affect both treatment and supervision experiences. Today's effective supervisors work to understand these dynamics and weave multicultural awareness throughout the supervision process.
Psychotherapy supervision's role as a vital educational practice has gained more international recognition now than ever before in its 100-year history. This worldwide acknowledgment shows how essential supervision has become in various therapeutic contexts.
How supervision supports ethical and effective practice
Supervision fulfills three key functions that promote ethical and effective practice:
Normative function: Ensuring quality control, monitoring supervisee treatment efforts, and safeguarding patient care
Formative function: Facilitating supervisee development, improving treatment knowledge, and developing conceptual/treatment skills
Restorative function: Encouraging emotional processing, attending to well-being, and preventing burnout
The restorative aspect has become more important as mental health providers face increasing workplace demands. Studies show 21-67% of mental health providers report experiencing burnout during their careers. Regular supervision gives practitioners emotional support that helps prevent isolation and burnout while encouraging self-care.
Clinical supervision acts as an ethical safeguard to help therapists direct complex ethical dilemmas. Supervisors' gatekeeping role includes protecting the public by ensuring new practitioners demonstrate competence and ethical practice. This oversight prevents potential ethical missteps, particularly during therapists' earliest development period—known to be challenging due to increased supervisee vulnerability.
Studies show supervision improves professional development at every career stage. Supervision continues to positively influence development even among senior practitioners, with research showing favorable connections between supervision and sense of growth. Positive supervision also relates to therapists' experience of "Healing Involvement" in their client work.
Supervision's effectiveness relies heavily on organizational support. Therapists who find their work settings satisfying, supportive, and conducive to good therapeutic practice often report more positive developmental supervision experiences. This shows how institutional factors substantially affect supervision quality.
Clinical supervision keeps developing while ethical considerations remain essential. Client confidentiality, consent, and professional boundaries need constant attention—especially given digital communication and remote supervision's complexities.
What clinical supervision actually looks like
Clinical supervision takes many forms behind closed doors. It serves as both a collaborative learning environment and a protective space where therapists develop their skills. Classroom knowledge alone isn't enough - hands-on supervision bridges the gap to real-life application.
What is hands-on supervision?
Hands-on supervision combines direct observation, personalized feedback, and practical guidance from experienced clinicians. This approach is different from classroom instruction because it focuses on real cases and immediate challenges. Supervisors create safe, non-judgmental spaces where therapists can openly discuss cases and ask questions without fear of criticism.
Hands-on supervision that works often has:
Learning about issues specific to patients that apply to clients of all types
Time set aside to discuss complex patients who need extra attention
Sessions that cover burnout prevention, countertransference, and feelings of professional inadequacy
Productive supervision relationships are built on regular meetings with clear communication and ongoing feedback. These sessions also set concrete goals that guide professional development and ensure quality client care.
Types of Supervision: What’s Right for You?
Not all supervision is created equal. Here are your main options:
1. Individual Supervision
One-on-one. Intimate. Focused. Great for diving deep into your caseload and exploring your clinical style. This support can feel the best for people, trust builds fairly quickly and allows for more time and attention.
2. Group Supervision
Think of it like a clinical potluck—you learn from others’ cases and perspectives. Want in? Join our Group Consultation »
3. Dyadic Supervision
Two supervisees, one supervisor. You get the benefit of shared learning and individual attention.
4. Peer Supervision
No boss, just peers. A great option for licensed clinicians looking for support and collaboration.
Helpful: Questions to Ask in Supervision
Supervision for therapists near me: how to find the right fit
The right supervisor won't appear overnight. Pre-licensed therapists in agency settings often get supervision as an employment benefit. Private practice therapists must look elsewhere.
Here's how to search for a supervisor:
Ask colleagues for referrals
Attend mental health networking events
Ask at local agencies or educational institutions
Search online mental health directories
The Clinical Supervision Directory connects supervisees with supervisors who have years of experience. A supervisor with expertise in your specialty area will add more value to your supervision. One therapist found their supervisor through a certification training that matched their focus on serving queer and polyamorous relationships.
Your supervisor-supervisee relationship needs careful consideration of several factors. Experts say compatibility with your learning style and professional goals tops the list of important criteria. Meeting potential supervisors helps assess qualifications and compatibility. Good supervision encourages your unique professional identity while ensuring ethical and effective client care.
The hidden mistakes supervision helps prevent
Common Supervision Pitfalls (and How to Avoid Them)
Even great clinicians (and supervisors) can slip into these traps:
❌ Too Much Theory
Clients don’t speak in acronyms. Focus less on the textbooks and more on the real talk.
❌ No Structure
Winging it? Not helpful. A simple agenda can change everything.
❌ Avoiding Tough Talks
Hard conversations are part of the job. Supervision should be a safe space for honesty.
❌ Forgetting Client Outcomes
Supervision should always connect back to how clients are doing. Don’t lose sight of that.
Learn more: How to Choose a Therapist Supervisor
Supervision Prevents 4 Major Career Killers
Let’s break them down:
1. Burnout & Isolation
Burnout is real. Supervision creates space for venting, reflecting, and reconnecting.
2. Ethical Blind Spots
No one’s immune to ethical slips. Supervision helps catch issues before they become problems.
3. Skill Stagnation
Without feedback, we flatline. Supervision keeps your toolbox growing.
4. Overconfidence Without Feedback
We all think we’re “above average.” Supervision keeps us grounded.
Therapist burnout and isolation
Mental health professionals face heavy emotional demands in their work. Research shows that 21-67% of mental health providers experience burnout during their careers. This psychological exhaustion can demonstrate itself through physical symptoms like headaches and sleep problems. Behavioral symptoms include irritability and negative attitudes.
Supervision offers a vital antidote to these challenges. Regular meetings with supervisors create a safe space where therapists can express their frustrations and process their emotional responses to clients. This prevents emotional exhaustion from building up. Studies show an inverse relationship between supervision quality and burnout - the risk increases by a lot when supervision is poor or missing.
The protection runs deep. Quality supervision gives three times the protection against burnout compared to those who lack proper supervisory support. This restorative role becomes more important as caseloads grow and emotional demands increase.
Ethical blind spots and legal risks
Good intentions don't shield therapists from ethical dilemmas that just need outside viewpoints. Supervision works as both risk management and ethical protection. Therapists might unknowingly participate in boundary violations, confidentiality breaches, or problematic dual relationships without proper oversight.
Poor supervision carries serious legal consequences:
Supervisors might face vicarious liability for supervisee misconduct
Ethical missteps can lead to lawsuits, criminal charges, or professional penalties
Poor documentation creates legal vulnerabilities
New therapists often miss these risks. Most residents think lawsuits will happen in medical practice, but none believe they'll face personal liability for training mistakes. Regular supervision helps spot these blind spots before harm occurs.
Stagnation in clinical skills
Professional growth depends on continuous learning and feedback. Therapists risk skill stagnation without supervision - they stay in fixed patterns instead of expanding their therapeutic toolkit. Clients experience this as being "stuck in a negative feedback loop".
Supervision fights this tendency by promoting ongoing professional development, which protects against professional stagnation. Therapists can identify countertransference issues, understand their limitations, and develop strategies to manage clinical work's emotional demands through guided self-examination.
Overconfidence without feedback
Overconfidence poses the most subtle threat to therapeutic effectiveness. The "better-than-average effect" guides most clinicians to believe they have greater skill than they actually possess. This natural cognitive bias creates danger when therapists act on hunches rather than evidence-based approaches.
Overconfident clinicians show clear patterns:
Commission: they act instead of reflecting
They give too many unsolicited suggestions to clients
They present interpretations as facts despite incomplete evidence
They rationalize mistakes instead of learning from them
Regular supervision deflates these inflated self-assessments through audio recording review and honest feedback. John Steinbeck captured this well-worded truth: "And now that you don't have to be perfect, you can be good".
How to make supervision more effective
Image Source: American Counseling Association
Clinical supervision can become a powerful tool for development instead of just another task when you plan and implement it strategically. Even experienced therapists benefit from guidance to get the most out of their supervisory experiences. Here's how you can improve clinical supervision through careful planning and execution.
Setting clear learning objectives
Learning goals often remain unclear to both supervisees and supervisors without specific objectives. A roadmap for professional growth emerges when you set specific learning targets rather than having unfocused discussions. Learning objectives should target measurable skills, knowledge, or attitudes that you can assess through direct observation.
Effective objectives serve multiple purposes:
They guide technique development and assessment
They make evaluation processes transparent
They help design specific teaching activities for supervision
Short-term and long-term objectives work together to balance immediate needs with future development. A short-term goal might include completing cultural competence training within a month. A long-term objective could target becoming skilled at culturally responsive interventions over a year.
Supervisors who share learning objectives with supervisees early in their relationship reduce anxiety about evaluation by a lot. This openness creates a collaborative atmosphere where everyone understands what success looks like.
Using outcome measures to guide sessions
Client feedback data in supervision sessions produces measurable benefits. Studies show that trainees who discussed client feedback during supervision were more satisfied compared to those who didn't. This feedback offers a "value neutral" foundation to discuss case progress.
Outcome measures serve as powerful tools by:
Helping practitioners detect symptom worsening
Revealing information that might go unnoticed
Keeping the client's voice central to the process
Supervisors should take a collaborative conversational approach with outcome measures instead of treating them as just numbers. This approach turns outcome data from paperwork into valuable clinical tools that boost engagement from practitioners and patients.
Encouraging honest feedback from supervisees
Giving and receiving feedback needs both parties to be open. Supervisees value feedback more from someone they see as a role model. Supervisors should welcome feedback too, which creates an environment where everyone learns.
These approaches help build honest communication:
Make it safe to discuss challenges without judgment
Build trust through consistent support
Give specific, timely feedback about behaviors rather than personality
Cultural competence is vital for effective feedback exchanges. Supervisors need cultural awareness training to support diverse supervisees effectively. This knowledge helps them understand how their worldviews connect with their supervisees' views.
Join our Group Consultation if you want to improve your supervision through shared learning. Multiple viewpoints can enrich your supervisory experience and show you effective feedback models.
Good feedback should be complete, prompt, honest and useful—not vague, unclear or surprising. This approach turns supervision from a routine task into a catalyst for professional excellence.
Common pitfalls in supervision and how to avoid them
Supervisors, even experienced ones, often fall into predictable traps that reduce their clinical supervision effectiveness. Both parties can make better use of their time together when they spot these common pitfalls early. This approach helps keep client outcomes as the main focus.
Too much theory, not enough practice
Many clinical supervision sessions turn into theoretical discussions about case formulation instead of addressing what happens during therapy sessions. Supervisors spend too much time looking at cases through various theoretical frameworks rather than exploring deeply into therapy's conversational nature. Carl Rogers made a crucial point in 1939: "A full knowledge of psychiatric and psychological information, with a brilliant intellect capable of applying this knowledge, is of itself no guarantee of therapeutic skill".
Supervision becomes more effective when it focuses on actual session recordings. Role-playing challenging clinical scenarios and practicing specific interventions help therapists implement new skills with their clients right away.
Lack of structure or agenda
Supervision sessions become ineffective without proper planning. Research shows supervision loses its value when it becomes a "tick box" exercise or too bureaucratic. Supervisees might not gain much from sessions if their supervisor shows up without an agenda. This behavior sets a poor example by suggesting that planning doesn't matter.
Sending agendas before meetings sets a good example of time management and helps supervisees prepare better. Starting each session with a collaborative agenda ensures focused discussions.
Avoiding difficult conversations
Staying silent about concerns can get pricey. Organizations that foster a culture of silence face communication breakdowns that hurt patients. A study revealed that while more than four out of five nurses worried about dangerous shortcuts, incompetence, or disrespect, less than half spoke to managers about their biggest concerns.
Supervisors need to build an environment where everyone feels comfortable having tough conversations about ethical dilemmas, performance issues, and personal reactions. Success depends on creating psychological safety where both sides can share their vulnerabilities without fear.
Neglecting client impact
Some supervisors put too much emphasis on the therapist's experience and not enough on client outcomes. They waste valuable time on less important matters like giving compliments while ignoring up-to-the-minute progress monitoring data that should guide their discussions.
Good supervision uses client feedback data and outcome measures to keep discussions focused on improving client care. Moving from therapist-focused to client-focused supervision helps avoid treating these sessions like personal therapy instead of professional development.
Questions every supervisee should ask
Image Source: Leapsome
Your supervision experience works better when you ask yourself and your supervisor the right questions. You can improve your professional growth by taking an active role through self-reflection.
What are my current learning goals?
You should identify specific growth targets that match your career goals. The next step is to build a contractual relationship with your supervisor and outline clear goals and methods. This helps both parties focus their efforts on areas that will affect client care.
How do I know if I'm improving?
Real growth needs solid evidence to measure it. Studies show that supervisees feel more satisfied when they talk about client feedback during supervision. Looking at outcome measures gives you an unbiased way to check your progress.
What feedback do I need but haven't received?
Along with checking your own work, you should ask for feedback from your supervisor. Simple questions like "How am I doing?" and "How can I improve my performance?" work well. Yes, it is vital to hear constructive criticism for professional growth—even when it feels uncomfortable.
How can I better support my clients through supervision?
Before each session, think about questions like: "Which parts of my practice challenge me most?" and "How well do I keep my boundaries?". Join our Group Consultation if you want different views on complex cases—this shared environment shows you various approaches and builds your clinical reasoning skills.
Conclusion
Clinical supervision is the life-blood of therapeutic practice, even though statistics about its effect on client outcomes remain puzzling. Our exploration shows that supervision does much more than what outcome studies can measure. Of course, good supervision helps prevent therapist burnout, spots ethical blind spots, curbs professional stagnation, and challenges the dangerous overconfidence that develops without regular feedback.
Therapy's changing landscape requires supervision to adapt. New technology, cultural changes, and complex clinical cases have revolutionized supervision from simple mentorship to evidence-informed practice. The pandemic has sped up these changes, making online supervision both common and essential.
Quality supervision needs intentional structure rather than casual case discussions. Clear learning objectives, outcome measures, honest feedback, and consistent focus on client impact should become standard practice. Without these elements, supervision becomes a box-ticking exercise that doesn't protect or develop practitioners.
Supervision's restorative role needs special focus. Mental health providers face heavy emotional demands, so supervision's support becomes vital for sustainable careers. This emotional support leads to better client care through therapists who stay present and engaged instead of burning out.
Both supervisors and supervisees must actively participate. The value comes from the questions asked, feedback sought, and vulnerability shared. Supervisees should own their professional growth by stating clear learning goals and asking for constructive feedback.
Research might not deal very well with measuring supervision's direct impact on client outcomes, but its value goes way beyond the reach and influence of statistics. Supervision protects and encourages growth, keeping therapists safe from common pitfalls while encouraging professional development. Best of all, supervision creates a space where therapeutic work can improve continuously—helping both therapists and their clients.
👇 Ready to Get Started?
Explore Supervision Services »
Join Group Consultation »
Key Takeaways
Despite research showing minimal direct impact on client outcomes, therapist supervision remains crucial for preventing hidden professional pitfalls and ensuring ethical practice.
• Supervision prevents four critical mistakes: therapist burnout and isolation, ethical blind spots and legal risks, clinical skill stagnation, and dangerous overconfidence without feedback.
• Quality supervision provides three essential functions: normative (quality control), formative (skill development), and restorative (emotional support and burnout prevention).
• Effective supervision requires structure and intentionality: clear learning objectives, outcome measures to guide sessions, and honest bidirectional feedback between supervisor and supervisee.
• Active participation maximizes supervision value: supervisees must ask targeted questions about learning goals, progress measurement, needed feedback, and client support strategies.
• Modern supervision adapts to evolving challenges: incorporating telehealth delivery, multicultural awareness, and technology integration while maintaining focus on client impact over theoretical discussions.
The hidden value of supervision lies not in measurable client outcomes but in its protective function—preventing professional isolation, ethical missteps, and skill stagnation that could ultimately harm both therapists and their clients. When structured effectively with clear objectives and honest communication, supervision transforms from routine obligation into a powerful catalyst for professional excellence.
FAQs
Q1. Why is therapist supervision important if it doesn't directly improve client outcomes? While research shows minimal direct impact on client outcomes, supervision is crucial for preventing therapist burnout, addressing ethical issues, promoting skill development, and providing emotional support. These benefits indirectly contribute to better client care.
Q2. What are the main types of clinical supervision? The main types of clinical supervision are individual supervision (one-on-one), group supervision (3-6 supervisees with one supervisor), dyadic supervision (two supervisees and one supervisor), and peer supervision (colleagues learning from each other without a designated supervisor).
Q3. How can supervisees make the most of their supervision sessions? Supervisees can maximize their supervision by setting clear learning objectives, preparing questions in advance, actively seeking feedback, discussing client outcome measures, and being open to constructive criticism. Taking an active role in the process is key to professional growth.
Q4. What are some common pitfalls in clinical supervision? Common pitfalls include focusing too much on theory rather than practice, lack of structure or agenda in sessions, avoiding difficult conversations, and neglecting client impact. Recognizing and addressing these issues can significantly improve the effectiveness of supervision.
Q5. How has the COVID-19 pandemic affected clinical supervision practices? The pandemic has accelerated the adoption of telehealth and telesupervision, allowing for greater flexibility and access to services. Supervisors now need to assist supervisees with unique challenges arising from virtual therapy and adapt their practices to accommodate remote supervision.
If you are interested in working with one of the supervisors at VitalMinds. Click link below to get started.