The Difference Between Supervision and Consultation (and Why You Might Need Both)
Mental health professionals have always needed supervision as a basic part of their training and skill maintenance. Most of us in the field know that both supervision and consultation help us grow, but the boundaries between these two support systems often get fuzzy.
Clinical supervision creates an intensive relationship where experienced professionals guide newer ones to build their knowledge and skills. Clinical consultation works differently - it's more of a peer-based or expert interaction that helps us throughout our careers. The difference between consultation vs supervision in counseling matters a lot in practice. Clinical supervisors must take legal responsibility for their supervisees' work, but consultants don't share this burden. These differences matter because new therapists need supervision to get licensed, while consultation serves other purposes at different career stages.
Client welfare remains our main goal as we direct our professional growth. We need to know exactly when to seek supervision, consultation, or both to improve our clinical skills and client outcomes. This holds true no matter how experienced we become.
What Is Supervision and What Is Consultation?
Mental health professionals often mix up supervision and consultation terms. These represent two different professional relationships that serve unique purposes and lead to distinct outcomes. Mental health professionals at every career stage should know these differences.
Definition of Clinical Supervision
Clinical supervision creates a formal, deep relationship between an experienced professional (supervisor) and a less experienced one (supervisee). The relationship has a clear hierarchy and evaluation components. Professional sources describe supervision as "a disciplined, tutorial process wherein principles are transformed into practical skills". Supervisors take professional responsibility to oversee their staff's clinical work and remain legally and ethically accountable for client care.
Supervision in counseling serves two main goals: It ensures quality client services and helps practitioners grow professionally. Regular feedback, evaluation, and performance reviews are part of clinical supervision. This long-term relationship acts as a gateway for new professionals entering the field.
Supervision helps turn theoretical knowledge into clinical skills through ongoing structured guidance. Supervisors hold administrative control and legal responsibility for their supervisees' actions, which sets this relationship apart from others.
Definition of Clinical Consultation
Clinical consultation works differently as a voluntary process between professionals with no hierarchy. Caplan and Caplan define consultation as "a process of interaction between two professionals–the consultant, who is a specialist, and the consultee, who invokes the consultant's help in a current work problem".
Consultants might have specialized knowledge but don't take direct responsibility for care implementation. Consultees can freely accept or reject suggestions, which makes consultation more collaborative than directive.
Practitioners ask for consultation when they face challenging cases, ethical dilemmas, or specific clinical practice issues. They can get consultation individually or in groups, regularly or as needed. Consultation maintains an equal relationship where status differences come only from the "authority of ideas" rather than organizational structure.
Why the Difference Matters
The difference between supervision and consultation goes beyond words, it carries real practical, legal, and ethical meaning:
Legal Responsibility: Supervisors are legally liable for their supervisees' actions. Consultants stay independent from such responsibility. This shapes how both relationships work and what guidance they provide.
Power Dynamics: Supervision naturally involves evaluation, but consultation doesn't. This power gap affects how people give and receive feedback and how they participate in the process.
Professional Development: Supervision helps advance careers, especially for license candidates. Consultation supports skill development throughout one's professional journey.
Decision-Making Authority: Consultees keep full control over clinical decisions. Supervisors can direct their supervisees' actions when needed.
These differences help practitioners choose the right professional relationship at different career stages. New professionals need formal supervision for licensing, but experienced practitioners benefit from consultation for complex cases or specialized expertise. Regulatory bodies also have specific rules about supervision that don't apply to consultation.
Both approaches help professionals grow and serve clients better, though they work through different relationships and methods.
Structural and Relational Differences
Mental health practitioners experience fundamental differences between supervision and consultation. These differences shape how relationships work in practice and go beyond basic definitions.
Power Dynamics: Hierarchical vs Peer-Based
Supervisors have positional power over supervisees in an unequal relationship. Bordin explained this as an "inescapable tension associated with status difference" in supervisory relationships. A supervisor takes on multiple roles:
Acts as the profession's gatekeeper by making sure supervisees meet standards
Protects the public as their primary duty
Serves as a professional conduct role model
Takes responsibility for supervisee's work
Supervision works through two main goals. It helps junior members grow professionally while keeping client care quality high. Bernard and Goodyear point out that supervision is "evaluative, hierarchical, extends over time and has the simultaneous purpose of enhancing the professional functioning of the junior member while monitoring the quality of services provided to the clients."
Consultation works differently. It happens between colleagues or peers without hierarchy. Consultants don't take responsibility for client care. Consultees can choose whether to use the advice they receive. This key difference lets consultees decide how to use the guidance they get.
Frequency and Format of Meetings
Supervision follows strict scheduling rules. Many jurisdictions require at least one hour of individual, face-to-face supervision weekly. Group supervision usually allows no more than eight people. Supervisees must complete 52 weeks of individual supervision during their training.
Rules state that professionals can't count more than six hours of supervision in one week. This shows how regulated the relationship is. Supervision continues until someone meets their licensure requirements.
Consultation happens when needed throughout someone's career. It might be a one-time thing or happen regularly based on specific challenges. Many professionals see consultation as part of their growth. They start with structured supervision as students, then move to mentorship, and finally clinical consultation as they gain experience.
Documentation and Evaluation Requirements
Supervision needs detailed documentation such as:
Written contracts that spell out expectations, goals, and responsibilities
Regular progress reports about supervisee growth
Formal evaluations with measurable performance criteria
Yearly assessment of strengths and limitations
Records of supervision hours for licensure
Supervisors must also watch and assess the "extent, kind, and quality of counseling performed by the supervisee." They do this through direct observation, recordings, or case note reviews. This evaluation part makes supervision different from consultation.
Consultation documentation stays simple. It usually just needs a written agreement about fees, time frame, and the consultant's expertise. Since consultants don't evaluate, they keep minimal formal records. They focus on specific clinical issues instead.
These structural differences help professionals choose the right approach at different career stages.
Legal and Ethical Responsibilities
Legal and ethical aspects create two distinct frameworks that separate supervision from consultation in mental health practice. These frameworks define professional responsibility and accountability differently.
Supervisor Liability vs Consultant Independence
The biggest difference between these roles lies in their liability gap. Supervisors face both direct and vicarious liability for their supervisee's actions. Direct liability happens when supervisors indirectly cause unethical behavior through their supervisees. This could mean having trainees use inappropriate treatments or giving them tasks beyond their skill level. The legal doctrine of "respondeant superior" makes supervisors accountable for supervisee actions through vicarious liability, even if they did nothing wrong.
Consultants work nowhere near the same level of oversight. Therapists just need specific feedback or advice from consultants, often in specialized areas like EMDR or DBT. So consultants don't carry the same legal responsibilities as supervisors. This creates two very different relationships. Supervisors deliver treatment through their supervisees without ever meeting the clients.
Many supervisors keep strict control over their supervisee's activities because of these liability differences. Some even limit which treatment methods supervisees can use based on their own training.
Regulatory Requirements for Supervision
Supervisory relationships must follow extensive regulatory requirements that consultation doesn't need. Twenty-four jurisdictions require supervisors to get pre-approval from their licensing boards. Most states have specific qualifications:
Thirty-five jurisdictions set minimum experience requirements, with 27 states needing an average of 2.8 years of clinical practice experience
Twenty-eight jurisdictions require supervisors to finish specialized training before they can supervise others
Nineteen jurisdictions need continuing education specifically for clinical supervisors, averaging four hours each year
Supervisors must hold proper licenses in their profession across almost all states. Many states also need documented supervision contracts that outline parameters, responsibilities, evaluation methods, and confidentiality limits.
Record keeping becomes vital as supervisors must track supervision sessions, evaluation forms, and supervisee progress reports. These requirements exist to protect public health and safety through quality control.
Ethical Boundaries in Consultation
Consultants carry significant ethical responsibilities despite having less legal liability. Both supervision and consultation need clear professional boundaries to work well and maintain integrity.
Clear professional relationships form the basis of appropriate boundaries. Healthcare professionals should stay away from dual or multiple relationships with clients that risk exploitation. Consultants and supervisees should also agree on clear confidentiality expectations.
Confidentiality is the life-blood of ethical considerations. Both relationships need informed consent documents that spell out information sharing practices. Supervisors must explain how they'll discuss client information during supervision. Consultants must ensure their consultees get client consent before sharing any identifiable information.
These relationships are built on fiduciary duty - putting another's interests first. A psychologist's position of power automatically creates a fiduciary relationship where the client's best interests come first.
Consultation might seem to have more relaxed ethical boundaries than supervision. Yet both relationships must follow professional ethics codes that emphasize clear boundaries. These boundaries prevent harm and help clients feel safe.
When to Use Supervision vs Consultation
Your need for supervision or consultation, maybe even both, largely depends on your career stage, practice goals, and clinical work challenges.
Supervision for Licensure and Early Career
Regulatory bodies require supervision during a clinician's original career phase. The requirements typically include tracking clinical hours, getting regular feedback, and submitting documentation to get licensed. To name just one example, many states need supervisees to complete a minimum of 100 hours of face-to-face supervision among 1,000 hours of direct client contact. This relationship must happen within an agency, institution, or group practice setting to meet regulatory standards.
Early career practitioners find supervision valuable because it:
Develops skills through regular feedback
Helps navigate ethical dilemmas
Builds foundational clinical competence
Protects through shared liability during learning periods
Supervision acts as both a professional gateway and safety net that will give a new clinician proper skills before independent practice.
Consultation for Complex Cases and Specialization
Clinical consultation becomes more valuable as professionals advance. The sort of thing i love about consultation is its help with challenging cases that need specialized knowledge or a fresh viewpoint. Unlike supervision, consultation happens selectively, often as needed, and serves different purposes:
Practitioners ask for consultation when they:
Work with challenging clients or unique presentations
Learn specialized treatment modalities like EMDR or DBT
Need extra viewpoints on ethical dilemmas
Build niche expertise or specialized services
Consultation makes shared space to review specific clinical questions, discuss diagnostic impressions, and plan treatments without shifting client care responsibility.
Ongoing Use of Both Throughout Career
The difference between supervision and consultation blurs throughout a professional's career path. Many clinicians use both relationships at once for different reasons. Consultation might happen less often but continues through one's professional life. Supervision often evolves into mentorship.
Experienced professionals join peer consultation groups that offer mutual support, decrease isolation, and create continuous learning chances. These groups work best in non-hierarchical, non-evaluative, yet honest settings.
Regulatory bodies encourage regular clinical consultation even after meeting licensure requirements. This ongoing connection with supervision and consultation helps practitioners maintain ethical standards, grow professionally, and deliver better client outcomes throughout their careers.
Benefits of Each Approach
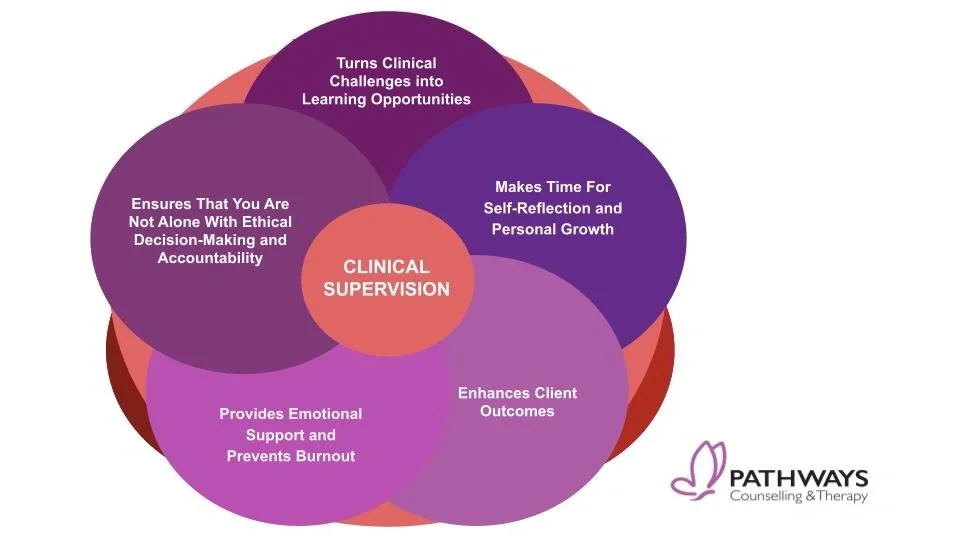
Supervision and consultation each bring unique benefits that boost different aspects of clinical practice, beyond their structural and legal differences. Clinicians can utilize both relationships to maximize their professional development by understanding these advantages.
Skill Development Through Supervision
Supervision is the life-blood of building foundational clinical competence. Regular, structured interactions with supervisors provide direct feedback that shapes core therapeutic skills. Trainees find a safe space to practice new techniques before using them with clients.
Providers consider supervision as "the single most important contributor to their professional development," which shows how much it affects their career path. The bond between supervisor and trainee creates the psychological safety needed for trying new clinical approaches.
The competency-based supervision model clearly shows what knowledge, skills, and values build clinical competence. Supervisees can focus their self-assessment on specific growth areas while supervisors can give targeted feedback. This approach makes goals clearer and helps create a better working relationship.
Case Insight and Peer Support in Consultation
Consultation brings fresh views to tough cases. Many clinicians describe it as "outsider insight" that helps spot patterns they might miss. Clinicians can review treatment approaches, explore diagnoses, and get specialized input without shifting client care responsibility.
Peer consultation helps reduce professional isolation - a key benefit for independent practitioners. Consultation groups create a supportive community of colleagues with shared experiences that provide both information and emotional support. These relationships help solve complex cases and ethical challenges together.
Clinical consultation helps identify blind spots in therapeutic relationships. Even seasoned therapists benefit from outside views that highlight relationship issues or treatment roadblocks they might miss.
Improved Client Outcomes from Both
Both supervision and consultation ended up improving client care. Research shows clear links between trainee skills, service quality, and better client outcomes. Effective clinical supervision drives treatment success.
Consultation helps therapists spot dysfunctional patterns in treatment, which leads to better client outcomes. When therapists participate in consultation, their clients show improvements in goal setting, competence, activation, self-efficacy, and self-care behaviors.
These approaches help clients get care from practitioners who constantly improve their clinical reasoning, expand their therapy tools, and stay professionally healthy. All these factors lead to more effective treatment.
Shared Goals and Overlapping Features
Supervision and consultation share basic goals that highlight how they complement each other in clinical practice, despite their different structures. These approaches focus on better client care by building professional skills.
Focus on Clinical Growth and Competence
Supervision and consultation help turn theory into real clinical skills. Quality client services and professional development are the main goals that bring these relationships together. Both relationships help practitioners make better clinical decisions beyond just managing cases. Clinical growth comes through structured learning opportunities, though they look different in each context. Supervision uses a more formal competency-based approach, while consultation tackles specific clinical challenges as they come up. Both methods show that better skills directly relate to treatment success, client retention, and how satisfied practitioners feel.
Supportive Feedback and Mentorship
Mentoring sits at the heart of supervision and consultation. Good supervisors and consultants lead by example and create safe spaces where people can learn. Strong relationships in both settings need:
Mutual trust and respect
Clear communication channels
Useful, constructive feedback
Recognition of strengths while working on growth areas
Mentoring starts formally in supervision and naturally shifts to consultation as practitioners gain experience. These relationships work best when they encourage self-reflection and help develop professional identity through open dialog.
Encouragement of Ethical Practice
Both supervision and consultation are crucial spaces where ethical practice develops. Supervision gives practitioners a place to learn ethical judgment, analysis, and decision-making. Consultation groups are a great way to get perspective on ethical challenges. These settings help clinicians see the differences between professional ethics, core values, and personal beliefs. Through support and guidance, clinicians learn to spot ethical issues, work through value conflicts, and use proper ethical reasoning, skills they'll need throughout their careers.
Conclusion
The difference between supervision and consultation helps us make better choices about our professional development needs throughout our careers. These two relationships might look similar at first glance, but they serve different purposes while sharing a common goal to boost client care and clinical competence.
Supervision creates a structured foundation that new professionals need. This hierarchical, evaluative relationship will give us core competencies and helps meet licensure requirements. On top of that, it makes supervisors legally responsible for our work. This creates a safety net as we direct ourselves through clinical practice complexities. Such oversight protects both new practitioners and their clients during this learning period.
Consultation takes a different approach by offering flexible, peer-based support that works at all career stages. We can ask for targeted guidance without evaluation when facing challenging cases or developing specialized expertise. This lets us keep our clinical autonomy while learning from others' wisdom and experience.
Many professionals find value in using both relationships at once. Supervision provides structure and accountability, while consultation offers specialized input and collegial support. Our professional trips need different types of guidance as we progress. We need complete oversight through supervision early in our careers. Later, the focused, specialized guidance of consultation becomes more valuable.
Both approaches emphasize ethical practice, clinical competence, and professional growth. That's why supervision and consultation stay essential throughout our careers. These are complementary relationships that boost different aspects of our professional development rather than competing approaches.
Supervision and consultation ended up serving the same vital purpose - they help us provide the best possible care while growing as practitioners. The real question isn't about which approach works better. It's about which one fits our current professional needs. Sometimes we need a mentor, sometimes a colleague. Knowing when to use each type of relationship shows our professional maturity.
Key Takeaways
Understanding the distinction between supervision and consultation empowers mental health professionals to make informed decisions about their professional development needs at different career stages.
• Supervision is hierarchical and legally binding - Supervisors bear legal responsibility for supervisees' actions, while consultants maintain independence with no direct liability for client care.
• Early career requires supervision, ongoing practice benefits from consultation - Supervision is mandatory for licensure with structured requirements, while consultation provides specialized guidance throughout your career.
• Power dynamics fundamentally differ between approaches - Supervision involves evaluation and authority over decisions, whereas consultation maintains peer-based autonomy where you choose whether to implement advice.
• Both relationships enhance client outcomes through different mechanisms - Supervision builds foundational competence through structured feedback, while consultation offers fresh perspectives on complex cases and specialized expertise.
• Documentation and regulatory requirements vary significantly - Supervision demands extensive record-keeping and formal evaluations, while consultation requires minimal documentation and fewer regulatory constraints.
The most successful practitioners often utilize both relationships simultaneously, leveraging supervision's structure and accountability alongside consultation's flexibility and specialized input to maximize their professional growth and client care quality.
FAQs
Q1. What are the key differences between supervision and consultation in mental health practice? Supervision involves a hierarchical relationship where the supervisor is legally responsible for the supervisee's actions. Consultation is a non-hierarchical, peer-based interaction without legal liability. Supervision is typically required for licensure and early career development, while consultation can occur throughout one's career for specialized guidance.
Q2. How do the power dynamics differ in supervisory versus consultative relationships? In supervision, there's an inherent power imbalance with the supervisor having authority over the supervisee's clinical decisions. Consultation maintains a more balanced dynamic where the consultee retains full autonomy in implementing advice. This affects how feedback is given and received in each relationship.
Q3. When should a mental health professional seek supervision versus consultation? Supervision is essential for early-career professionals working towards licensure, providing structured skill development and meeting regulatory requirements. Consultation is valuable throughout one's career, especially when facing complex cases, seeking specialized expertise, or desiring peer support without the evaluative component of supervision.
Q4. What are the documentation requirements for supervision compared to consultation? Supervision requires extensive documentation, including contracts, progress reports, formal evaluations, and tracking of supervision hours. Consultation typically involves minimal documentation, usually just a basic agreement outlining the parameters of the relationship. This reflects the different legal and regulatory obligations of each approach.
Q5. How do supervision and consultation contribute to improving client outcomes? Both supervision and consultation aim to enhance client care, but through different mechanisms. Supervision builds foundational clinical competence through structured feedback and skill development. Consultation offers fresh perspectives on challenging cases and access to specialized expertise, helping practitioners refine their approach to complex clinical situations.
If you are interested in working with one of the supervisors at VitalMinds. Click the link below to get started.